62 year old male with CKD
Final exam short case
19/01/2023
Chief complaint :
A 62 year old male patient of resident Eluru dist, farmer by occupation came to casuality with the chief complaints of decreased appetite, vomiting, nausea, facial puffiness, pedal edema, and decreased urine output from 15 days.
History of present illnesses:
patient was apparently Asymptomatic 10 years back then he developed fever, difficulty in having food and was taken to hospital and found that he had diabetes mellitus and he taken medication
Patient was again symptomatic 3 years back and he noticed pedal edema, facial puffiness and was not treated for it
And later 2 years back the patient was Unconscious and unable to talk and was presented to local Regional hospital and was diagnosed the condition as renal disease. And he taken medication for renal disease but was not controlled.
15 days back he was suffering from vomitings, nausea, facial puffiness, pedal edema, distention of abdomen, decreased urine output, decreased appetite.
No history of SOB, chest pain, pain abdomen
History of past illness:
Known case of hypertension since 1 year and on medication tab.
Nicardia 10mg
Known case of diabetis mellitus since 10 years and is on medication
( Insulin injection )
Not a known case of epilepsy,asthma and Tb
Personal history :
Diet :mixed
Appetite :decreased
Bowel and bladder movements :irregular
Micturation:burning micturation
Allergies :no allergies
Addictions : Bidi smoking 5 years back (1packet per day)
Family history :
Not significant family history
Daily routine :before 15 days
6:00 am wake up
7:00-8:00 am breakfast (upma ,Dosa ,Rice sometimes)
9:00 am went to work
1:00-2:00 pm lunch(Rice, dal, vegetable curries ,non veg occasionally)
6:00 pm return to home
7:30- 9:00 pm dinner (Rice , chapati with vegetable curries)
10:00 sleep
General examination:
Patient is consciousness, coherent, cooperative and well oriented to time, place.
Patient is moderately built and nourished
Pallor:absent
Icterus:absent
Clubbing:absent
Lymphadenopathy :absent
Pedal edema :present
Vitals :
Bp:170/90mm Hg
Temperature : afebrile
Pulse rate :69bpm
Respiratory rate:15 cycles per minute
Systemic examination:
Cvs:
Inspection:
Chest is bilateral symmetrical
No visible engorged veins, scars or sinuses on chest
Palpation:
S1 and S2 are heared
No thrills or murmurs
Apex beat present at 5th intercoastal space 2cm lateral to mid clavicular line
Auscultation:
No cardiac murmurs heard
Respiratory system:
Inspection:
Chest is normal, bilateral symmetrical
Position of trachea is central
Movements are bilateral symmetrical
No scars, sinuses or visible pulsations
Air entry in bilateral
Palpation :
All inspectory findings are confirmed
No local rise of temperature
No tenderness
Percussion:
Right. Left
Supraclavicular Resonant. R
Infraclavicular. R. R
Mammary. R. R
Axillary. R R
Infra axillary. R R
Suprascapular. R R
Interscapular. R R
Infrascapular R R
Auscultation:
Normal vesicular breath sounds
Abdomen:
Distention of abdomen
No tenderness
No palpable mass
Liver and spleen not palpable
CNS:
patient is conscious
Speech is nornal
No neck stiffness
Investigations :
2D echo
USG abdomen
Complete urine examination
Blood grouping
Hemogram
Blood urea
Serum creatinine
Serum electrolytes

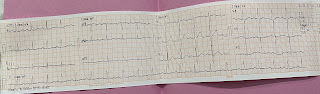
ECG :
provision diagnosis:
Chronic kidney disease
Diabetic nephropathy
Hypertension since1 year
Treatment:
Tab Nodosis 500mg po/bd
Tab nicardia retard 10mg po/od
Tab shelcal po/od
Inj iron Salt restriction less than 1-2 grms per day
Inj monosef 1grm iv bd
Tab baclofen 5mg po tid 100mg+100ml normal saline iv once in a week













Comments
Post a Comment