60 yr old male with SOB
A 60 years old Male with SOB
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome. I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 60 year old Male came (on 18/10/22)with
c/o cough since 6 days
C/o SOB since 6 days
HOPI-
Pt was apparently asymptomatic 1 year back Then he had fever with thrombocytopenia,from then he started having SOB ,was admitted in hospital and got treated
Now after 1 year pt complaints of
Cough with sputum which is white in color ,mucoid,non foul smelling,non blood stained
Cough is more during night
C/o SOB since 3 months
SOB increases on lying down
Grade-
Palpitations +
Sweating +
A/w fever
Past history:
N/k/c/o HTN,DM,Asthma,Epilepsy ,TB
H/o surgery to spine
Personal history :
Diet mixed
Appetite normal
Bowel and bladder movements regular
Sleep disturbed (because of cough)
Smokes 9 beedis per day (since 50 years)
Smokes cigarette occasionally
Drinks toddy in summers
Drinks alcohol occasionally
Daily routine-
General examination
Pt is c/c/c well oriented to time ,place and person
Well built and nourished
No pallor,icterus ,clubbing ,generalised lymphadenopathy
Vitals on admission -
BP-170/60mmHg
PR-50bpm
RR-32 cpm
CVS-
S1S2 +
Pan systolic murmur
JVP elevated
RS -
Inspection -
Trachea appears to be central
Pattern of breathing -abdominal
Shape of chest -barrel
Auscultation-wheeze +
CNS:higher motor functions intact
No focal neurological deficit
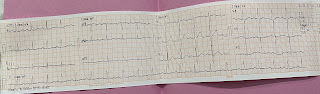
Investigations:
Serology-negative
FBS-78 mg/dL
PLBS-108 mg/dL
Blood urea -31
Serum creatinine-1.0
Hb-11.2 gm/dL
TLC-6,700
Neutrophils-57
Lymphocytes-33
Eosinophils -1
Monocytes-9
Basophils-0
TP-5.9
Albumin -3.83
A/G-1.85
FBS-78
PLBS-108
HbA1c-6.4
Cxray-
18-10-22
PFT
Diagnosis:
COPD (chronic bronchitis >emphysema ) with right heart failure


Comments
Post a Comment